free shipping desktop
How Cold Weather Can Affect Foot Pain

As winter sets in, many of us start digging out our heavy coats and turning up the thermostat. But for those managing chronic foot or ankle issues, the drop in temperature can trigger a noticeable increase in aches, pains, and stiffness. You are not imagining it; there are physiological reasons why your feet hurt more when the mercury drops. From changes in blood flow to the viscosity of the fluid in your joints, winter weather is a common culprit for exacerbating musculoskeletal conditions.
In this article, we will explore the science behind why cold weather impacts your lower extremities and discuss practical strategies to keep your feet comfortable and healthy all season long.
Poor Circulation in Cold Weather: What it Means for Your Foot Health
One of the most immediate ways cold weather impacts your feet is through the circulatory system. When exposed to cold air, your body’s intelligent survival mechanism kicks in. It prioritizes keeping your core organs (like your heart and lungs) warm. To achieve this, the blood vessels in your extremities (your hands and feet) undergo a process called vasoconstriction. This narrowing of the blood vessels significantly reduces blood flow to the toes and feet.
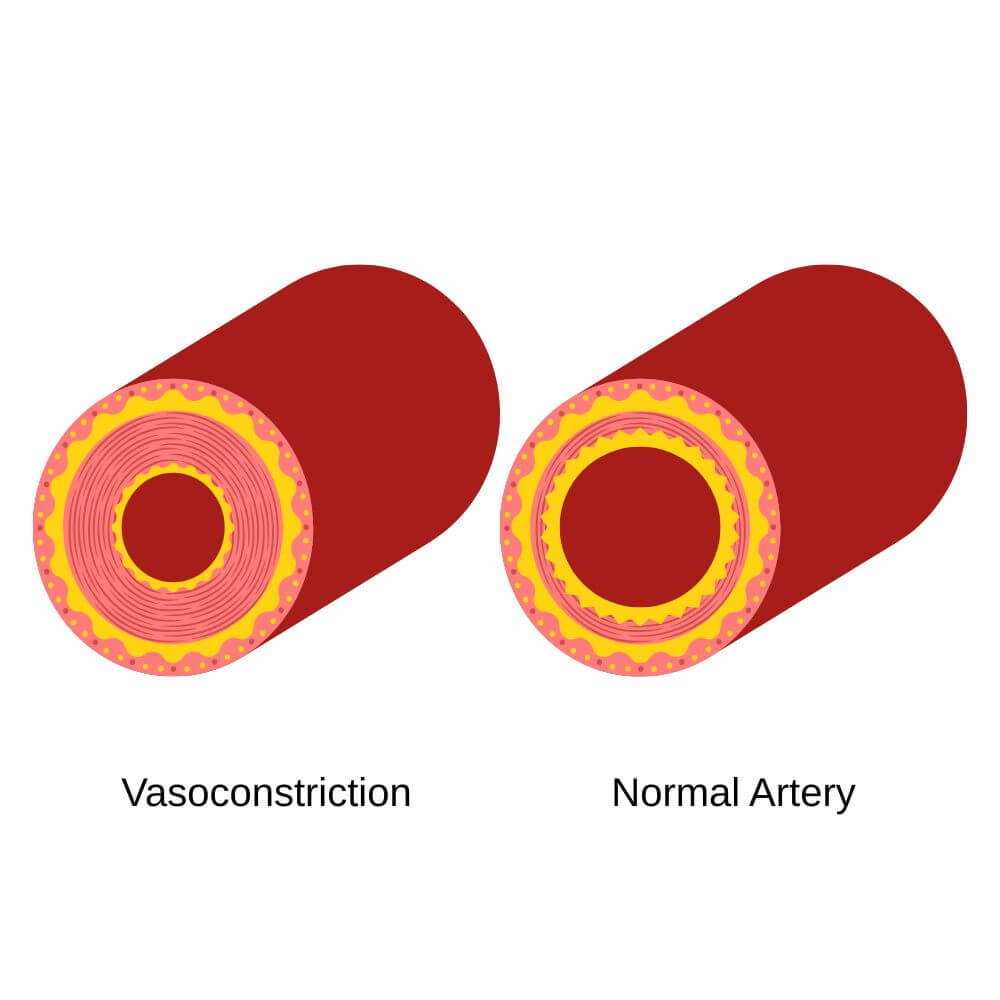
While this response helps maintain your core body temperature, it leaves your feet vulnerable. Reduced circulation means less oxygen and fewer nutrients are being delivered to the tissues in your feet. If you are recovering from an injury or managing a condition like tendonitis, this reduction in blood flow can slow down the healing process. Furthermore, for individuals with compromised circulation, such as those with diabetes or Raynaud’s, this vasoconstriction can be painful and potentially dangerous, leading to numbness, color changes, and tissue damage if not managed properly.
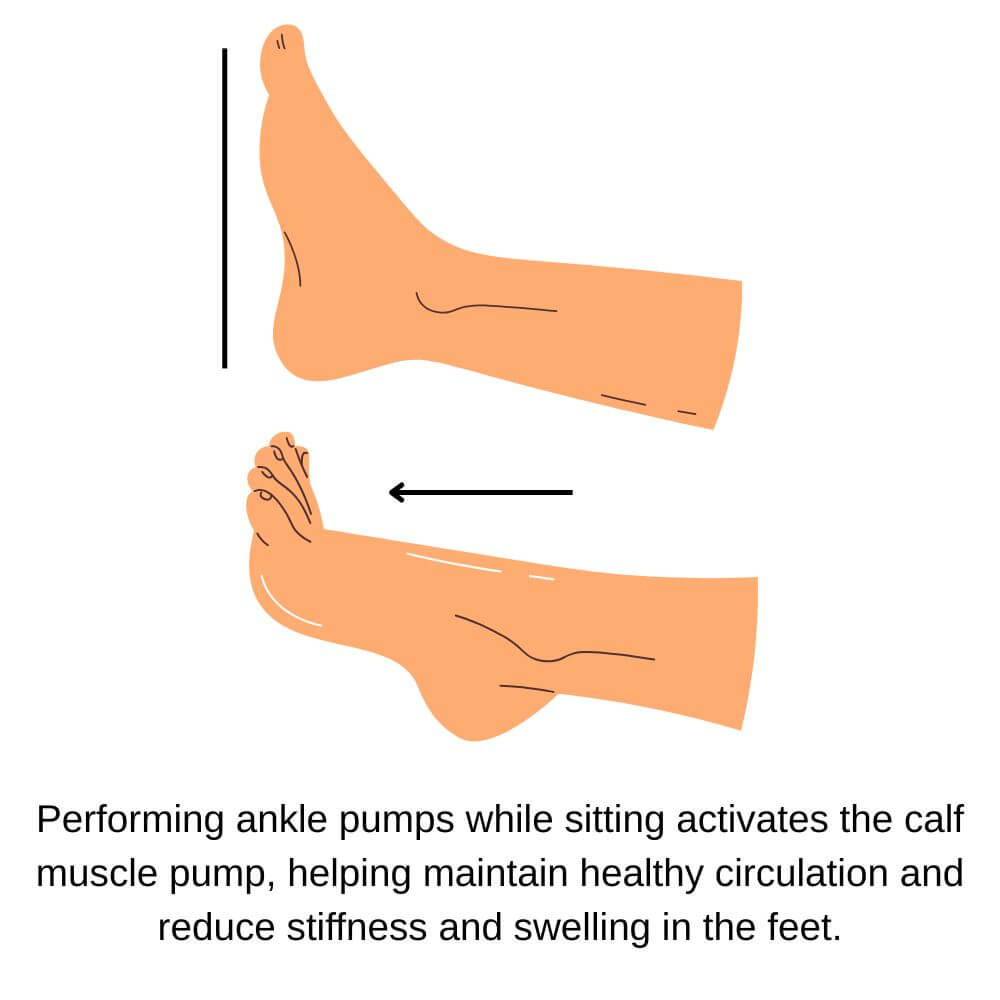
To combat this, it is vital to keep your core warm, not just your feet. Layered clothing helps maintain a regulated core temperature, preventing your body from aggressively shunting blood away from your feet. Additionally, active movement is key. Even simple ankle pumps or toe wiggles while sitting can encourage blood return and keep the vessels open.
Why Joints Feel Stiff and Muscles Ache in Cold Weather
Have you ever noticed that your body feels "creaky" on a freezing morning? There is a biological explanation for this sensation. Your joints are lubricated by a substance called synovial fluid. This fluid acts like motor oil in a car engine, reducing friction between the cartilage surfaces of your bones.
Research suggests that as the temperature drops, the viscosity (thickness) of synovial fluid increases. Think of it like trying to pour honey that has been in the refrigerator versus honey that has been sitting in the sun. Thicker synovial fluid creates more resistance within the joint capsule, making movements feel stiffer and requiring more energy to perform.
Simultaneously, cold temperatures cause your muscles and connective tissues to contract and temporarily lose elasticity. This tightening puts additional tension on the tendons and ligaments in your foot and ankle. For someone with muscle, tendon, or ligament impairments in the foot or ankle, this cold-induced contraction can increase the stress on these structures, potentially causing discomfort for some, particularly for those with existing conditions.
Dynamic warm-ups are highly recommended any time of year before exercise, but are absolutely essential during the winter. Engaging in 5-10 minutes of light movement indoors before heading out into the cold prepares your synovial fluid, muscles, tendons, and ligaments for activity. Heat therapy, such as a warm soak or heating pad, can be used in conjunction with a dynamic warm-up to increase tissue pliability, but should generally not replace it.
Barometric Pressure and Arthritis: Why Winter Hurts More
Many patients tell me they can predict the weather based on the pain in their joints, and science backs them up. The culprit is often barometric pressure: the weight of the atmosphere pressing down on us. Winter weather systems are frequently accompanied by drops in barometric pressure.
When the pressure outside drops, the tissues within your body experience a relative expansion. In a healthy joint, this micro-expansion might go unnoticed. However, in an arthritic joint or an area with chronic inflammation, there is less space to accommodate this swelling. The expanding tissues can press against sensitive nerve endings, resulting in increased pain signaling.
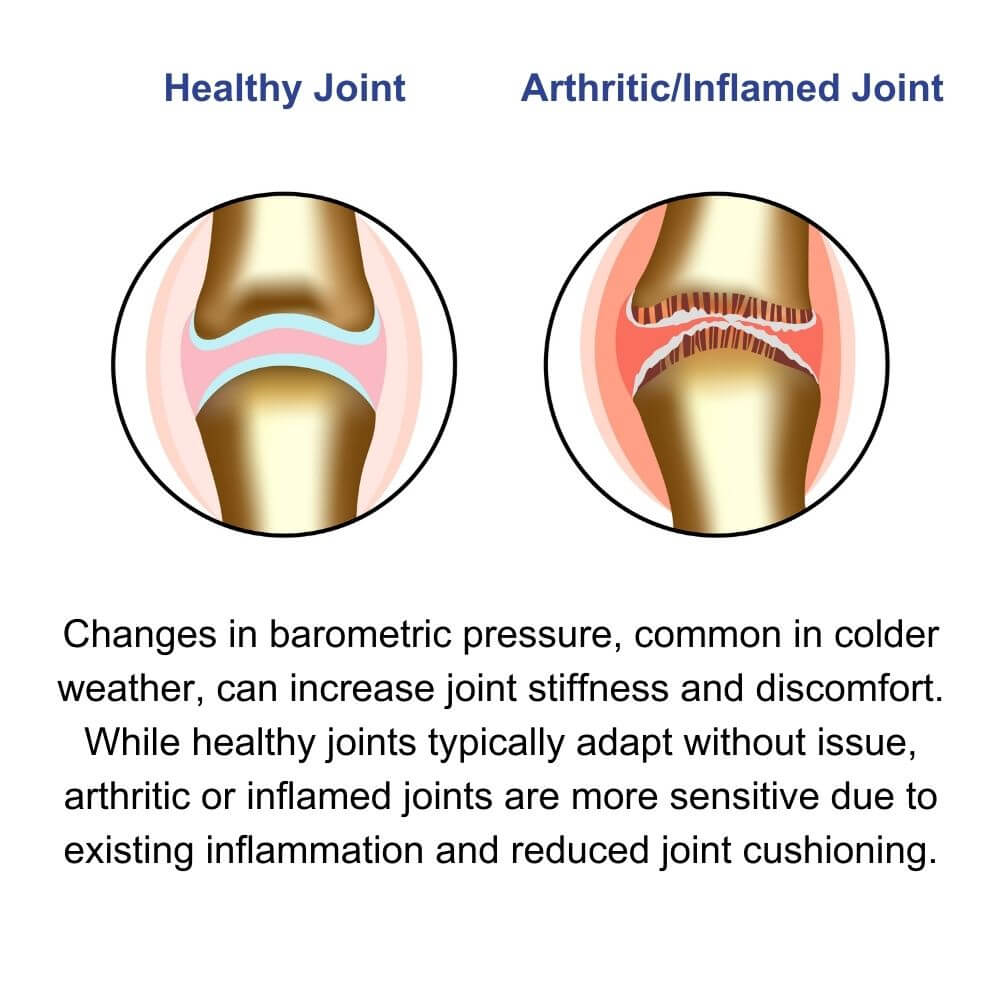
This phenomenon explains why "damp cold" often feels worse than "dry cold." The combination of low pressure and high humidity can cause tissues to swell just enough to irritate an already sensitive joint capsule, leading to that deep, aching throb associated with arthritis.
While we cannot control the weather, and moving south for the winter is not a feasible solution for most of us, compression socks can be a helpful tool here. They provide external pressure that may help counteract the swelling caused by barometric drops. Keeping a consistent routine of low-impact movement, like swimming in a heated pool or stationary cycling, also helps flush inflammation and maintain joint mobility despite the atmospheric changes.
Barefoot Indoors in Winter: What to Know
It is tempting to kick off your heavy boots the moment you get indoors. And for those with healthy feet and ankles, walking barefoot (or with socks) indoors is not only okay but can have some excellent effects on foot health. However, for those with pre-existing foot and ankle conditions or other conditions affecting the sensation of the feet, walking barefoot on cold, hard surfaces (like tile or hardwood) can be detrimental, especially in winter.
The "first-step pain" characteristic of plantar fasciitis is often exacerbated by cold floors. When your feet are cold, the plantar fascia (the thick band of tissue on the bottom of your foot) is tighter. Stepping directly onto a cold, unyielding surface may result in a more rapid stretch to less pliable tissue. For those with existing plantar fascia pathology, this can lead to increased pain.
Furthermore, cold surfaces can numb the sensory feedback from your soles. If you have neuropathy or reduced sensation, you might not notice how hard your heel is striking the ground, leading to bone bruises or stress injuries, along with increased risk of falling. For those with fat pad atrophy (thinning of the natural cushioning on the heel), the lack of insulation between bone and cold floor can be particularly piercing.
If you have an existing foot or ankle condition, talk to your doctor or physical therapist about whether you should adopt a "no barefoot" policy in the winter (or all year). Supportive house slippers or a dedicated pair of clean indoor sneakers can provide the necessary support and insulation. This protects your plantar fascia from shock and keeps the tissues warm and pliable throughout the day.
Winter Footwear: Choosing the Right Support & Protection
Finally, the shoes you choose to battle the elements play a massive role in your foot health. Unfortunately, many winter boots prioritize waterproofing over biomechanical support. A heavy, rigid boot can alter your gait, causing you to shuffle or drag your feet, which may put you at increased risk for compensatory overuse injuries.
Conversely, unsupportive fashion boots often lack a stabilizing heel counter or arch support. This can lead to your foot collapsing inward (often referred to as “overpronation”) inside the boot, which may also increase risk for overuse injuries, particularly to the posterior tibialis muscle and tendon.
Regardless of the type of winter footwear, another common issue is fit. We tend to wear thicker socks in winter, which can make our usual shoe size too tight. This compression can restrict circulation (the very thing we want to avoid) and compress the toes, which may lead to or exacerbate ingrown toenails or neuromas.
Lastly, the most obvious safety factor for those living in areas with snow and ice is traction. Not only is there the risk of injury due to falling on the ice, but regaining balance when you begin slipping requires your muscles to fire rapidly and forcefully to stabilize you. These sudden contractions can increase risk of musculotendinous injury, particularly to cold, less elastic tissues.
To combat these factors, look for these features when selecting winter footwear:

1. Removable Insoles: This allows you to replace the included insole with a higher-quality over-the-counter or custom orthotic for better support, alignment, and shock absorption.

2. Adjustable Closures: You should be able to loosen the boots using laces or straps to accommodate thicker socks without cutting off circulation, which can otherwise worsen cold sensitivity, numbness, or swelling.

3. Rubber Soles with Deep Lugs: Quality rubber compounds tend to stay flexible in freezing temperatures (unlike some plastics which harden and become slippery), and deep treads provide mechanical grip on snow or slippery terrain.
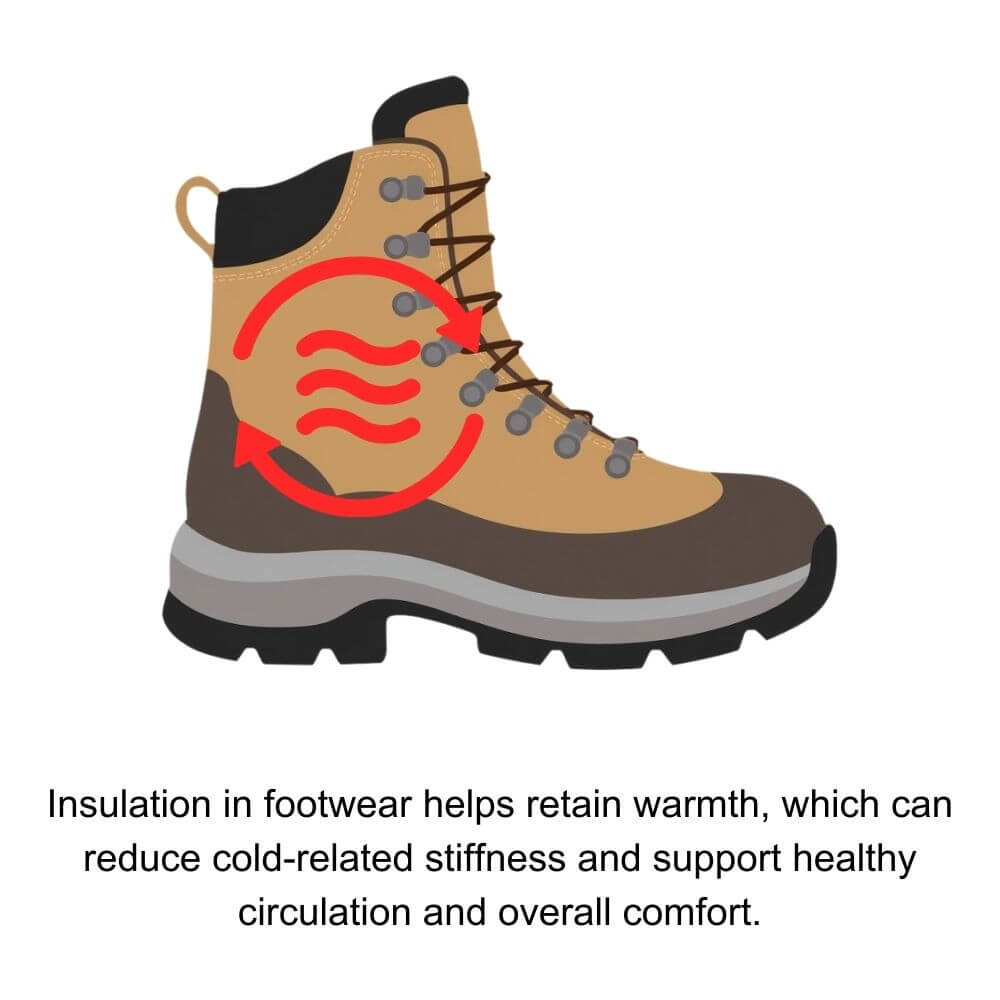
4. Appropriate Insulation: Look for materials like 3M™ Thinsulate (200g or more for cold climates) to maintain warmth without excessive bulk. Keep in mind that insulation needs vary based on activity level and circulation.

5. Adjustable Depth: Shoes with removable insole layers or double-depth construction allow extra room when needed, helping accommodate swelling that can occur during colder months from reduced circulation, prolonged sitting, or underlying conditions.
By understanding the physiological changes your body undergoes in the cold, you can take proactive steps to protect your feet. Winter doesn't have to be a season of increased pain; with the right knowledge and footwear, you can stay active and comfortable until the spring thaw.
About author:
Troy Hurst, PT, DPT, is a licensed physical therapist who received his Doctor of Physical Therapy degree from Carroll University in 2017. He specializes in the treatment of orthopedic and vestibular conditions, and has been a freelance medical writer since 2018.











