free shipping desktop
Can Your Foot Shape Cause Shin Splints?

Shin splints are a common lower body injury, particularly prevalent among runners and athletes in sports involving running. In fact, a study published in Cureus in May 2024 suggests that between 13.6% and 20% of runners have shin splints and the condition accounts for up to 60% of all lower limb injuries among this population.
While athletic populations may be the most susceptible to shin splints, the general population is not immune. The human body functions as a proverbial ‘chain’ with superior regions of the body affecting the alignment and movement patterns of the regions beneath it, and vice versa.
The cause of shin splints is often multifactorial and involves anatomical and physiological factors elsewhere throughout the body. We will discuss what shin splints are, why and how they occur, the role of foot structure, and some preventative or alleviating measures.
What are Shin Splints and Why Do They Occur?
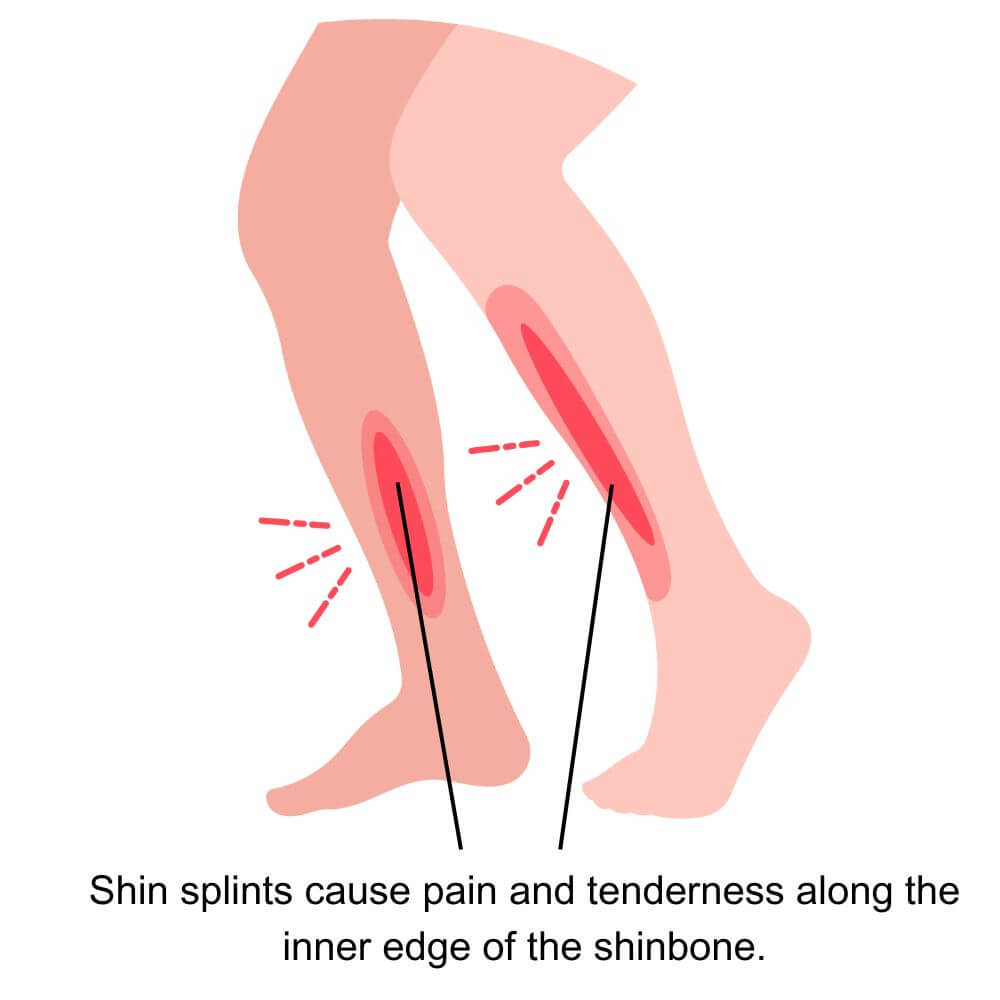
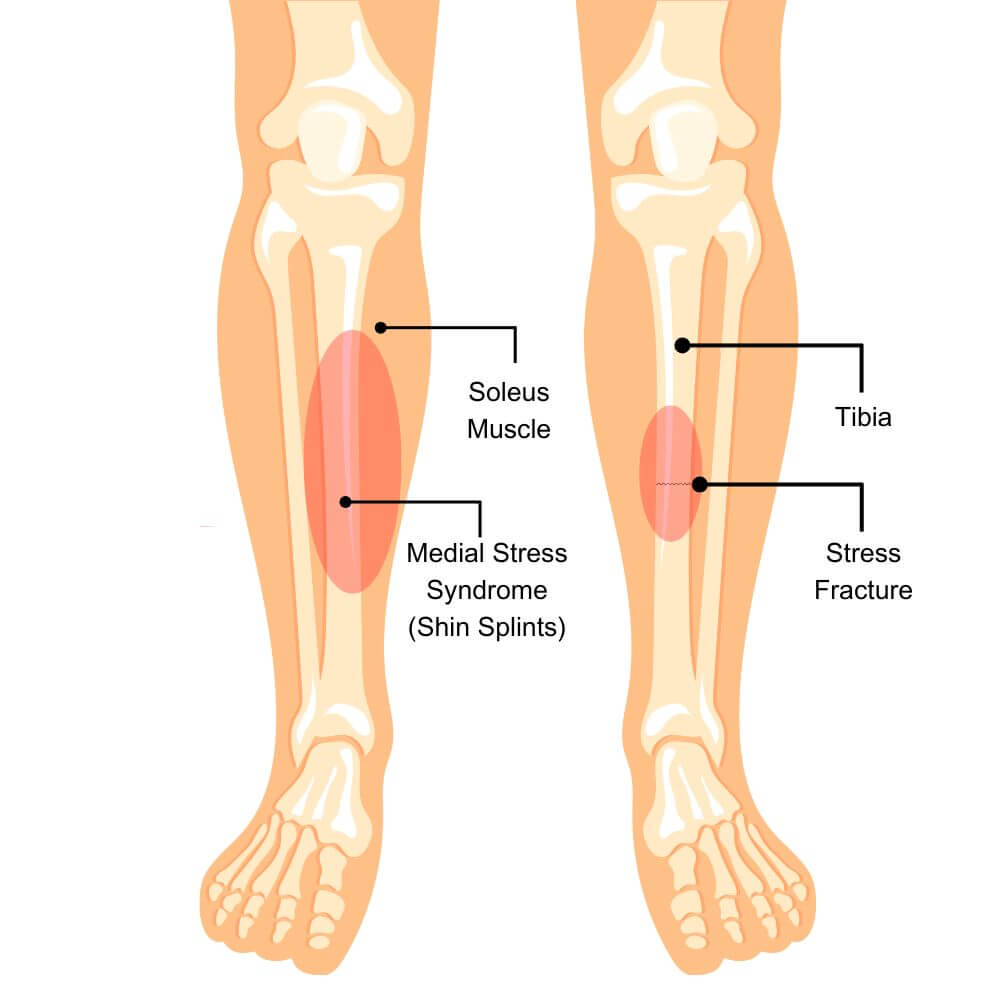
Shin splints, medically known as medial tibial stress syndrome (MTSS), refer to pain along the inner edge of the shinbone (tibia). This condition is most commonly experienced by athletes and individuals who engage in activities involving repetitive weight-bearing lower body impact. The primary symptom of shin splints is a sharp or throbbing pain along the medial (inside) portion of the shin. Symptoms occur most frequently during or after physical activity, however, the pain may persist even at rest, indicating more severe MTSS, or the potential risk of stress fracture or other more serious conditions.
The primary cause of shin splints is repetitive stress on the tibia and the connective tissues that attach the muscles that surround the tibia to the bone. This stress can lead to inflammation and microtears in the affected muscle and the outer layer of bone tissue. Commonly, shin splints are triggered by a sudden increase in the intensity, duration, or frequency of high-impact activities, meaning people doing “too much too soon” are the most likely to experience this condition. When it comes to athletes, particularly runners, a well-designed training (and recovery) plan is by far the most important preventative measure. Additionally, inadequate footwear is rarely the sole cause of the condition but can certainly exacerbate it.
Outside of the broader issue of training and recovery structure, the physiological reasoning behind overuse injuries, such as shin splints, involves body structures and tissues that have not adequately adapted to the stress being placed on them. For instance, every time you do something active that makes you just a little sore, your body triggers a chain of reactions to repair the microdamage of the affected tissues but will build them back up slightly stronger than they were before so your body can be better prepared to handle that amount of stress in the future. The process occurs very gradually, which is why you can’t safely go from running your first mile to running your first marathon overnight. If you provide a stimulus that is too much for what your body tissues have adapted to handle, you put yourself at much higher risk of overuse injuries because the microdamage we discussed before is no longer so micro, and your body can’t quickly and easily repair the amount of damage that was caused by the level of stress you placed upon it.
The Role of Foot Structure
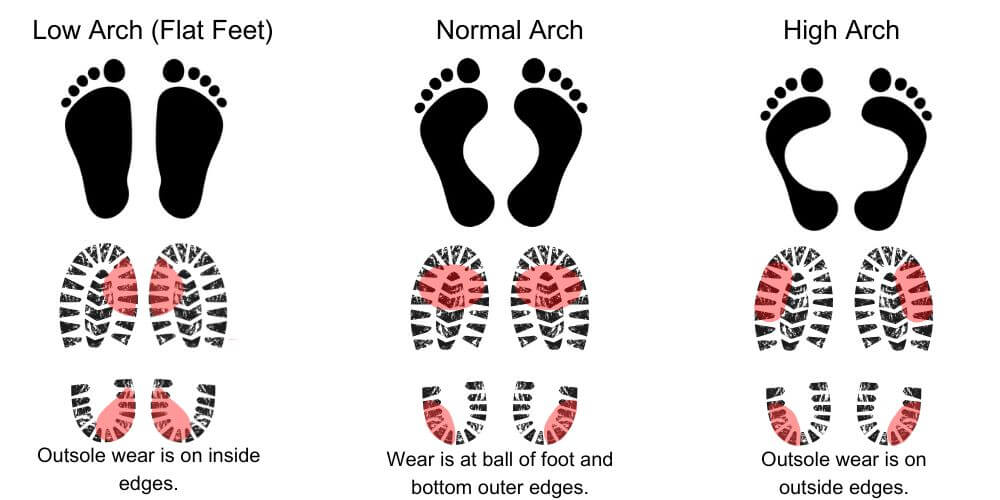
The anatomical structure and biomechanics of the feet also play a significant role in the development of shin splints. Individuals with flat feet or high arches are more prone to this condition due to the abnormal distribution of forces on the lower leg.
Flat feet can cause excessive pronation (commonly referred to as “overpronation”), where the foot rolls excessively inward when walking, leading to increased stress on the inside of the tibia. Conversely, high arches can result in excessive supination (AKA “underpronation” or “oversupination”), where the foot does not roll inward enough, causing a lack of shock absorption and increased impact on the lower leg. Both of these biomechanical issues can contribute to the development of shin splints.
Footwear Matters: Why Choosing the Right Shoes is Important
Proper footwear plays a key role in the prevention and management of shin splints. While more research is needed in determining optimal footwear structure and its impact on lower body injuries, current medical knowledge suggests that for those with flat feet (pes planus), high arches (pes cavus), or people who have active shin splints (or other impact-related overuse injuries), shoes that provide adequate structure, arch support, and cushioning based on the person’s foot structure and alignment are important in mitigating the impact forces exerted on the lower legs during weight-bearing activities.
For people meeting the criteria outlined above, proper arch support can assist in regulating the transfer of forces from the ground through the appropriate structures of the lower leg, thereby reducing the strain on the tibia and surrounding muscles. Cushioning absorbs shock and minimizes the repetitive stress that can lead to inflammation and microtears in the muscle and bone tissue.
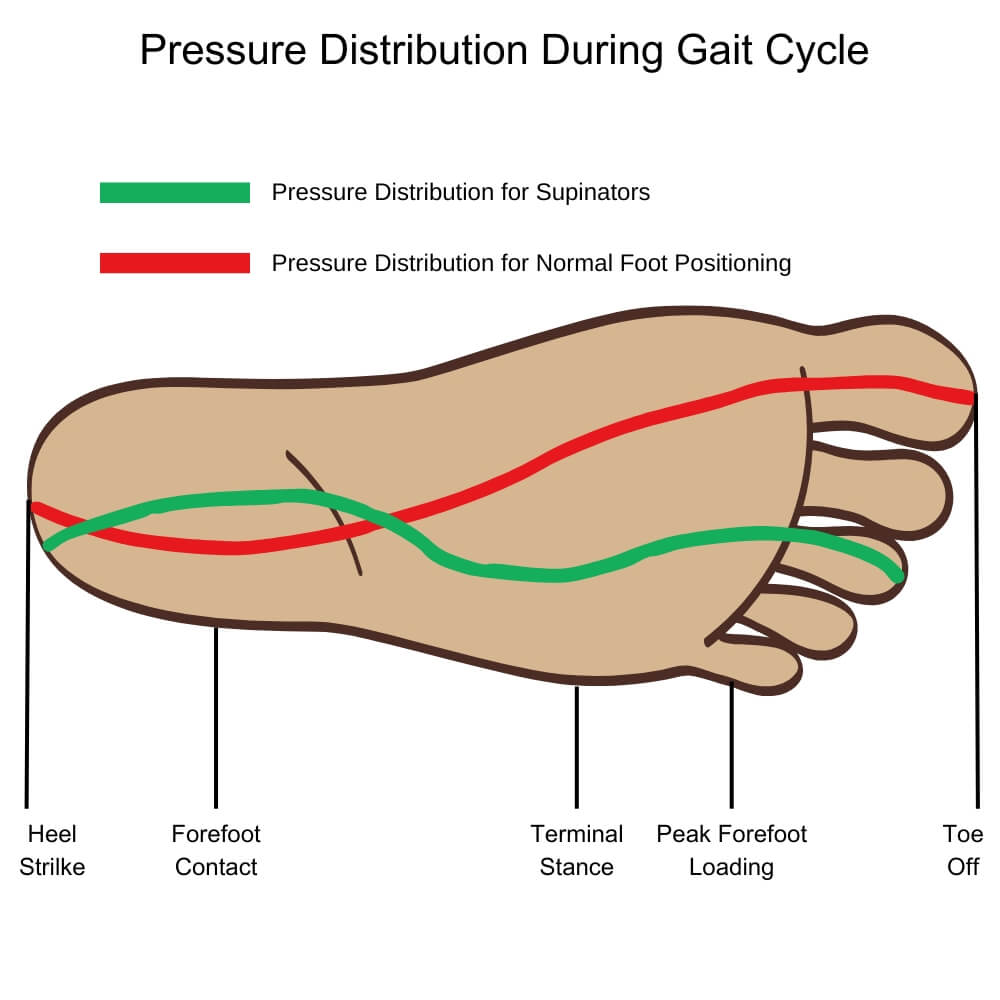
Worn-out or unsupportive shoes may exacerbate or contribute to the development of shin splints. Over time, the cushioning and support in shoes degrade, leading to decreased shock absorption and the potential for suboptimal foot and ankle biomechanics through the gait cycle (how you walking and distribute weight in each step), leading to poor force transfer. This can potentially increase the stress on the tibia and surrounding connective tissues, making individuals more susceptible to shin splints. It is important to regularly check the condition of athletic shoes and replace them when they show signs of wear and tear, such as flattened soles or uneven tread patterns.
For uninjured individuals with normal foot/ankle structure and biomechanics, this is still a highly debated topic that requires more research. Interestingly, current research suggests that the comfort of a shoe is the most important factor in injury prevention for this population.
When selecting orthopedic or specialty shoes to reduce the risk of shin splints, it is important to consider individual foot biomechanics. For those with flat feet, shoes with strong arch support and motion control features can help prevent overpronation and reduce stress on the medial tibia. Conversely, individuals with high arches should look for shoes with ample cushioning to enhance shock absorption and prevent underpronation. If you're experiencing persistent shin pain, a foot specialist, like a podiatrist or physical therapist, can help assess your needs for specific foot structures, contributing factors, and activity levels.
Custom Orthotics and Insoles: Do They Help with Shin Splints?
For some, utilizing orthotics inside a well-selected pair of shoes may be necessary to achieve the best results. Custom orthotics and over-the-counter (prefabricated) insoles can be beneficial in addressing foot structure issues that contribute to shin splints. These devices provide additional support and cushioning, helping to correct foot structure issues such as those discussed previously. By improving foot alignment and distributing forces more evenly across the lower leg, orthotics can reduce the stress on the tibia and surrounding muscles, thereby alleviating pain and preventing further injury.
Custom insoles are particularly helpful for individuals with unique or severe anatomical foot and ankle conditions that cannot be adequately addressed by over-the-counter options. For example, those with severe flat feet (pes planus) or high arches (pes cavus) may require personalized orthotics to provide the necessary support and biomechanical correction. Custom orthotics are designed based on a detailed assessment of an individual's foot structure and biomechanics, ensuring a precise fit and optimal functionality. On the other hand, over-the-counter insoles can be a cost-effective and convenient solution for individuals with mild to moderate anatomical foot and ankle conditions. These prefabricated insoles are available in various designs and levels of support, making it easier to find a suitable option for general use.
Incorporating custom orthotics or over-the-counter insoles into one's footwear may reduce the risk of shin splints, decrease exacerbation and pain levels in those who currently have shin splints, and enhance overall comfort during physical activities.
While your foot shape and structure are rarely the sole cause of shin splints, they can certainly be a contributor. If you believe you have shin splints or have a foot condition that is causing pain, balance deficits, difficulty moving safely or efficiently, or otherwise impacting your function, it’s important you speak to your doctor about it. If necessary, you may be referred to a podiatrist who can provide detailed, personalized recommendations based on your condition, provide footwear recommendations, and properly fit you for custom orthotics if needed.
About author:
Troy Hurst, PT, DPT, is a licensed physical therapist who received his Doctor of Physical Therapy degree from Carroll University in 2017. He specializes in the treatment of orthopedic and vestibular conditions, and has been a freelance medical writer since 2018.

