free shipping desktop
How Do High Arches Affect Your Feet and Lower Body?

The arches of your feet are often taken for granted but are formed by a complex array of anatomical structures that play a crucial role in the biomechanics of our gait. The importance of our foot arches is often not thought about unless you are born with or develop a condition that causes a deviation from the norm.
Those who do have conditions affecting their arches can readily tell you just how instrumental this small feature of our bodies is. Of the conditions affecting arch height, low arches, resulting in “flat feet” (also known as pes planus), gets significantly more attention. However, excessively high arches, also known as pes cavus, can be equally bothersome if not managed properly.
What Are High Arches and How Do They Form?

Pathologically high arches are known in medicine as “pes cavus,” which is Latin for “hollow foot.” Most people with severe pes cavus developed the condition from factors outside of their control.
Most people with true anatomical pes cavus are people with neurological conditions such as Charcot-Marie-Tooth disease, cerebral palsy, or spina bifida. For these individuals, management will be more aggressive, and preventative techniques obviously do not apply. Depending on the severity, surgical procedures may be necessary for these patients.
However, others have high arches that are less severe and may be due to either modifiable or non-modifiable factors. One common cause of high arches that is manageable but non-modifiable in terms of preventing the root cause is hereditary origin. Others develop pes cavus because of a foot or ankle injury that results in anatomical or compensatory changes that lift the arch beyond its optimal height.
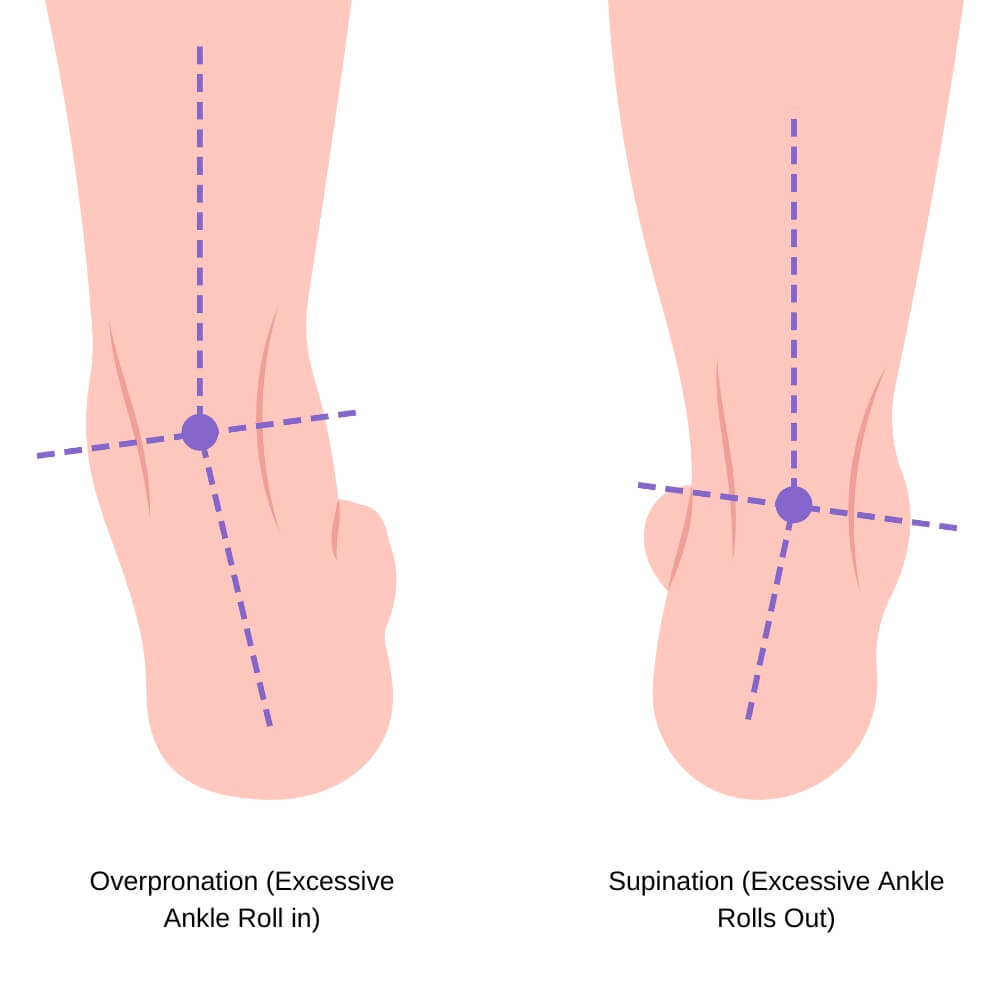
Commonly, we see a “false” pes cavus where there is not truly an anatomical change to a person’s arch height, but rather an overly supinated foot and ankle (or a lack of normal foot and ankle pronation) leading to an apparently high arch. This can be caused by numerous factors, many of which have to do with the alignment of the tibia (shin bone) as it articulates with the ankle.
One such example is for individuals with an acetabulum (hip socket) orientation that is pointed too far forward or backward, which leads to an overly internally or externally rotated femur (thigh bone), which then causes additional compensations and alignment issues at the tibia and ankle, resulting in an overly supinated foot. There are many other examples of anatomical alignment, short/hypertonic muscles, and joint mobility issues that lead to similar results.
How High Arches Impact the Feet (and the Rest of the Body)
With every step we take, the foot contacts the ground at the outer edge of the heel, our weight transitions over the foot as the rest of our foot meets the ground, and, at the same time, our foot and ankle pronate (roll slightly inward), allowing more of our arch to come in contact with ground before propelling forward with the majority of our weight translating over the first and second toes. This process of foot strike to ankle and foot pronation is crucial for proper propulsion and weight distribution when we walk.
High arches, or artificially high arches due to a lack of foot and ankle pronation, disrupt the normal gait process and prevent proper biomechanics. This may result in increased pressure points on the foot, decreased balance, decreased gait fluidity and speed, and increased stress on the surrounding structures of the foot, ankle, knee, and hip.
Due to the lack of normal pronation during the gait cycle, pes cavus will often result in pain in the heel, along the lateral (outside) edge of the foot, the 3rd-5th metatarsals in the middle and outside ball of the foot, and the 3rd-5th toes.

There is also an increased risk of hammertoes and claw toes, plantar fasciitis, recurring lateral ankle sprains, falls, and knee, hip, and low back pain as a result of the suboptimal gait mechanics.
The Role of Orthopedic Shoes for High Arches
Orthotic shoes can provide an effective form of management for many people with high arches. Their primary role is the redistribution of weight through the foot to both relieve the common pressure areas discussed above, as well as improve lower extremity alignment and biomechanics. This combination of factors ensures that both local and global symptom contributors are addressed.
Orthopedic shoes for high arches often feature midfoot support that promotes improved foot and ankle pronation through the gait cycle while redistributing weight across a wider surface area of the foot. Additionally, these shoes often incorporate a deep heel cup to better distribute pressure across the heel, as this is one of the most significant pressure points for people with pes cavus.
The shoes typically also offer a wide toe box to promote improved splaying of the foot during the gait cycle, which better distributes weight across the metatarsals and toes. This addresses another common set of pressure points while encouraging a more normalized toe-off while walking.
Other common features of orthopedic shoes for pes cavus include increased cushioning and stability features to reduce “hot spots” in the foot that often affect those with the condition, as well as a reduced risk of ankle sprains and falls.
When to Seek Medical Attention
If you have high arches and experience pain points in your feet that limit your ability to stand or walk for extended periods of time despite the use of comfortable footwear, you should speak with your podiatrist or primary care provider. Additionally, if you experience recurring ankle sprains or numbness, tingling, or shooting pain through your feet or toes, it is important that you consult with your doctor to address the underlying issues.
Pes cavus can be a multi-faceted condition that may occur for a wide variety of reasons, both orthopedic and non-orthopedic. As with most conditions, there is not a “one-size-fits all” cause or treatment protocol, and being evaluated by a medical professional will provide an accurate route for addressing your symptoms and their causes.
About author:
Troy Hurst, PT, DPT, is a licensed physical therapist who received his Doctor of Physical Therapy degree from Carroll University in 2017. He specializes in the treatment of orthopedic and vestibular conditions, and has been a freelance medical writer since 2018.

