free shipping desktop
Effective Ways to Relieve Pain on the Bottom of Your Foot

Pain in the sole (plantar surface) of the feet is one of the most common orthopedic conditions. In many ways, it makes a lot of sense that this is a hot spot for soreness, pain, and injury because the structures that support the natural arch of our feet must carry our full bodyweight every time we stand, walk, and run. With a relatively tiny surface area of our bodies responsible for such an important role, things can occasionally go awry.
In this article, we’ll discuss common causes of pain in the bottom of the foot, how to manage it, and when it may be time to have it addressed by a specialist.
Common Causes of Bottom of Foot Pain
As with any orthopedic pain, injury, or dysfunction, there can be multiple factors at play with plantar foot conditions. The feet are among the most elaborate anatomical structures of the entire body, as each foot contains 26 bones, 29 muscles, over a hundred tendons and ligaments, fascia, nerves, blood vessels, skin, bursa, and more.
The complexity and cohesive nature of the foot’s many structures are truly miraculous, but not fool-proof. With the feet being our connection point to the ground when we are upright, they regularly must support more weight than any other structure.
Some of the most common causes of pain in the bottom of the foot include:
Plantar Fasciitis
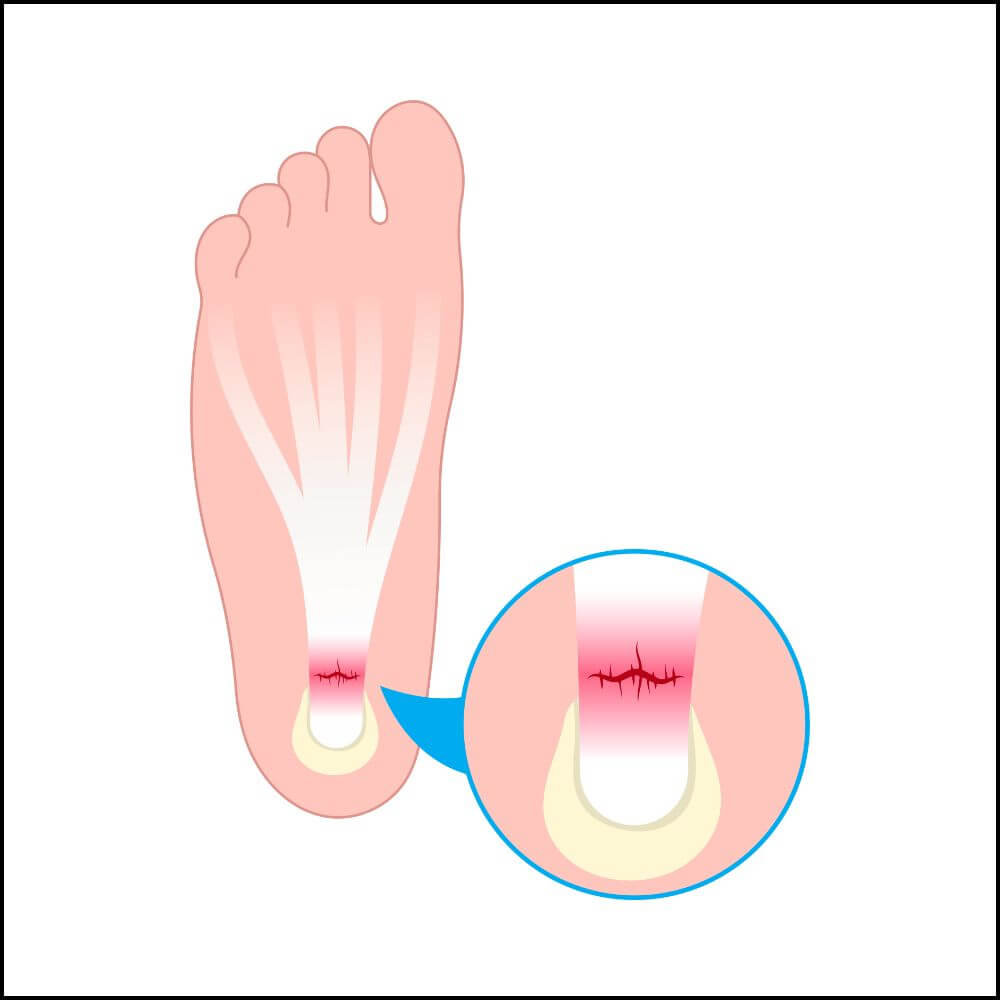
Plantar fasciitis is a condition that most people have heard of (or experienced) before. This condition encompasses inflammation of the fascia (connective tissue) along the bottom of the foot, which helps support our arch.
This condition can be either acute or chronic, and typically causes a sharp or stabbing feeling near the heel (where the plantar fascia originates) and along the sole of the foot. As with most forms of orthopedic tissue inflammation, the pain is often worse when the tissue is not warmed up, such as right away when you wake up in the morning and for the first several steps after you get up from sitting. It will typically improve as you get moving and get the blood flowing a bit more. It can also be quite painful when walking barefooted, particularly on hard floors.
Metatarsalgia (Ball of Foot Pain)
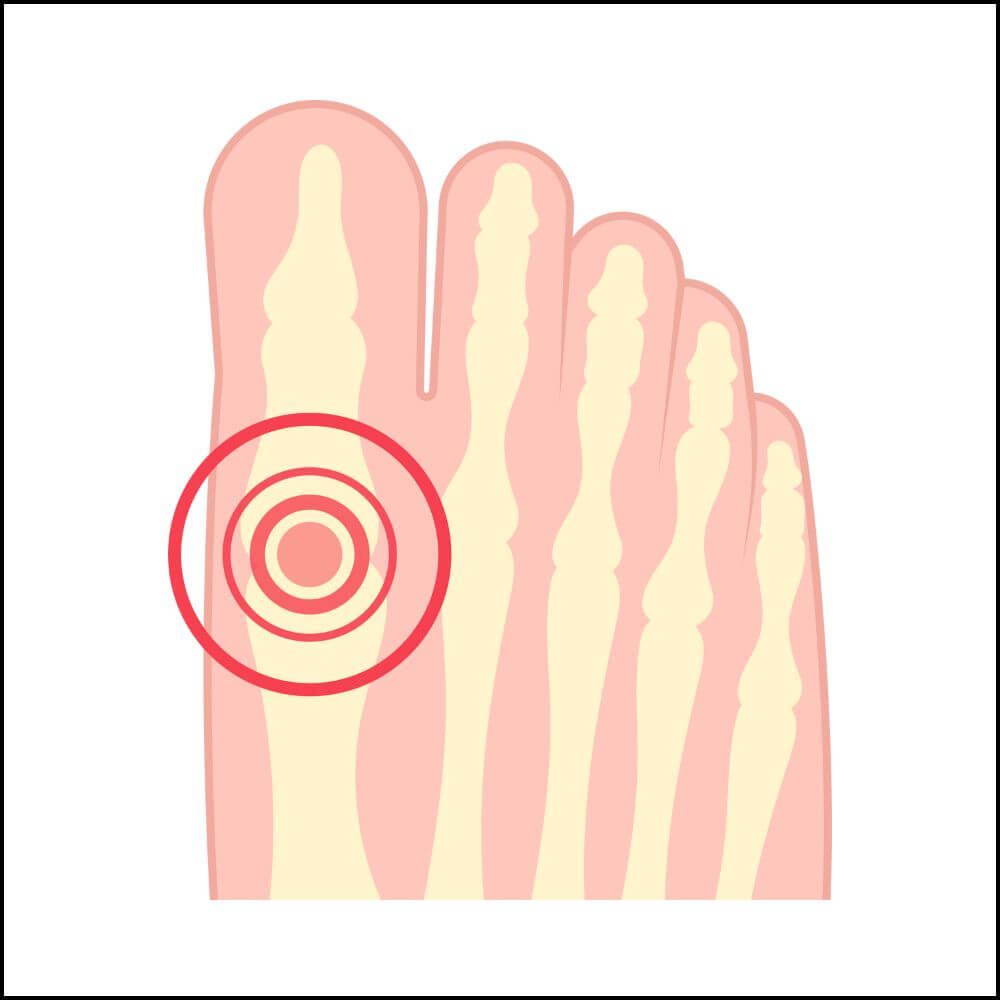
The metatarsals are long bones that run through the mid-foot and articulate with the tarsals towards the heel/ankle and the phalanges (toe bones). Since our weight transfers through the metatarsals every step we take, inflammation is common through these bones. Poorly fitting footwear and foot deformities are regular contributors to metatarsal pain as well.
Most of the time, pain through the metatarsals is temporary and uncomfortable at worst, but if you are experiencing severe pain that seems to linger at rest, this could be a sign of a metatarsal fracture (or stress fracture), and you should see you doctor as soon as possible.
Morton’s Neuroma
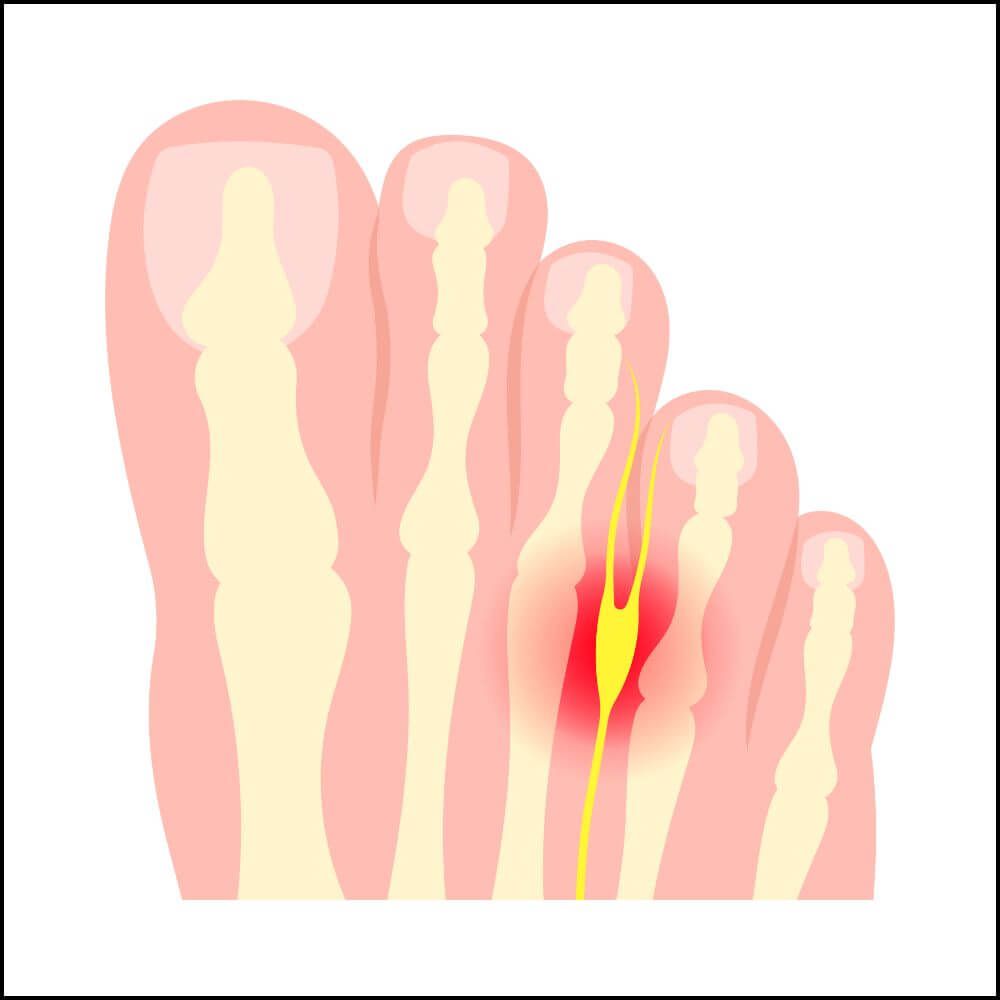
Morton’s neuroma is widely unknown outside of the medical field but is more common than you may think! This condition is a result of a thickening of the tissue around the tiny nerves that run between your toes (digital nerves). This can cause pain, discomfort, and numbness or decreased sensation in the bottom of your foot, typically between the toes.
Tarsal Tunnel Syndrome

As with Morton’s neuroma, tarsal tunnel syndrome is a condition that is caused by nerve compression and irritation. People with this condition have compression of their tibial nerve as it passes through the tarsal tunnel, which is a passageway on the inner side of the ankle.
Tarsal tunnel syndrome can cause pain, tingling, burning, and/or numbness in the foot, including the plantar surface.
Osteoarthritis
Most of us are familiar with osteoarthritis, and as with any other joint in our body, it can develop in the feet as well. Osteoarthritis affects millions of people around the world and is a result of degeneration of the articular cartilage at joint surfaces. When this occurs in the joints of our feet, it can cause pain through any area of the foot, including the bottom.
Osteoarthritis typically causes pain and stiffness, which is most pronounced right away in the morning or after periods of inactivity. Since it is a degenerative condition, it is much more common in older people.
Other Sources of Bottom of Foot Pain
Other common sources of plantar foot pain include overuse injuries, peripheral neuropathy, bursitis, and sesamoid bone pain. There are many other possible sources of pain not covered here, so if you have been experiencing nagging pain in the bottom of your feet, it’s always best to consult with your doctor.
How to Manage Bottom of Foot Pain
Many non-surgical management options are available for the conditions discussed above. Depending on the condition, multiple or all of these options may be incorporated to improve pain levels, mobility, and quality of life.
Lifestyle and Activity Modification
As with any injury, short- or long-term modification of your daily activities may be necessary to keep symptoms at bay. For plantar foot pain, this may include:
- Reducing time on your feet
- Avoiding uneven surfaces like uneven grass or dirt, crushed stone surfaces, or hiking trails
- Altering your exercise to avoid high-impact weight bearing activities like running or technical hiking
Exercises and Stretches for Bottom of Foot Pain
The best exercises and stretches for plantar foot pain are highly dependent on the root cause of a person’s condition. Therefore, there is not a single set of exercises that is best for all plantar foot pain. However, for those conditions in which the pain is localized to the bottom of the foot and not radicular pain from a nerve or a blood vessel, the following exercises and stretches are a good place to start:
Arch Lifts (Foot Doming)
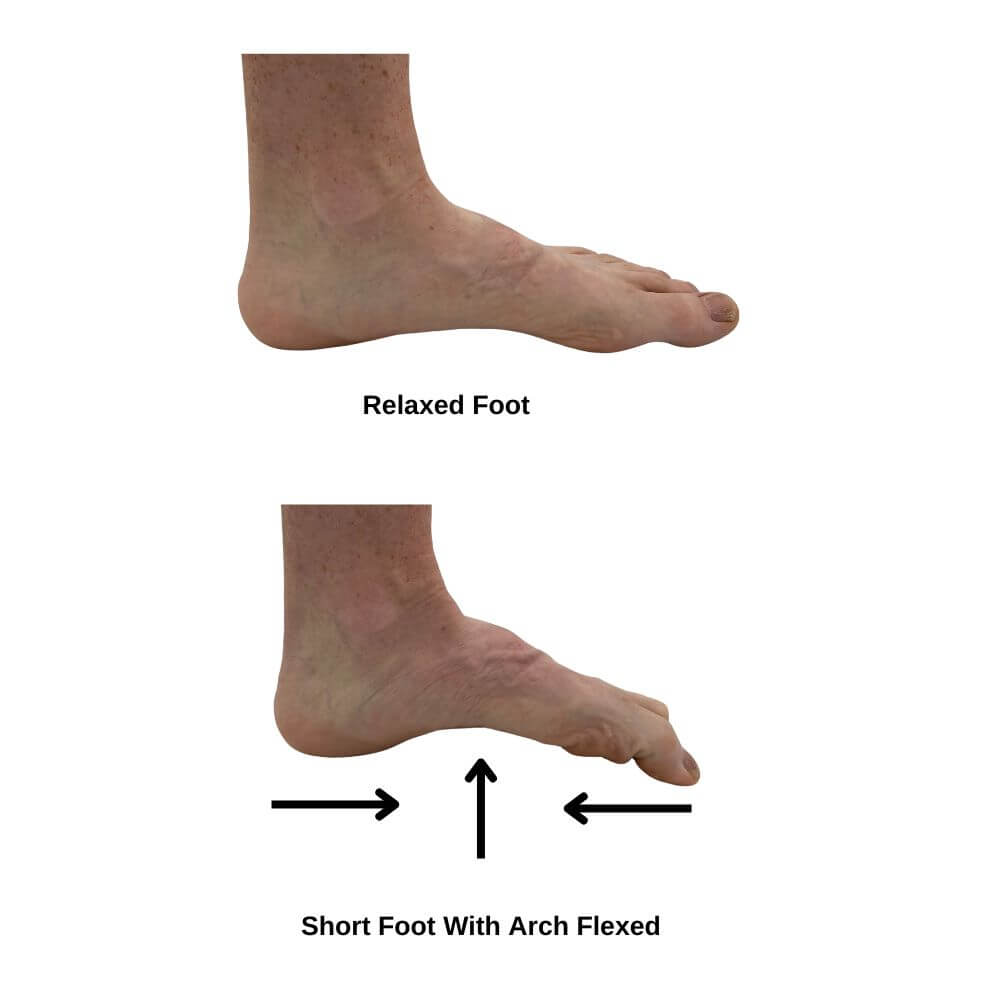
Arch lifts can be performed in sitting or standing and involve keeping the heel and toes in contact with the ground while using the intrinsic foot musculature to lift the arch of the foot up. Hold the contraction for 5-10 seconds before relaxing. Complete the desired number of sets and reps based on your current condition. The key is to avoid gripping the ground with your toes, as this will not provide the desired effect.
This exercise strengthens the muscles that support your arch (the intrinsic foot muscles) which can lead to improved arch height for those with flat feet, as well as improved foot mechanics while walking.
Seated Plantar Stretch

This stretch involves sitting with one leg crossed over the other knee. One hand is used to hold the ankle in place, while the other is used to gently pull the toes and foot backward until a stretch is felt in the bottom of the foot and the calf. The stretch should feel light to moderate intensity, but never painful. Hold for 30 seconds to one minute.
Plantar Foot Roll

This exercise can be performed with a small ball (such as a golf ball, tennis ball, or lacrosse ball), a small massage roller, or a frozen water bottle (which serves a double function by also reducing inflammation). This can be performed sitting or standing with the foot on top of the ball, roller, or water bottle. Gently roll the middle of the foot forward and backward over the ball, roller, or water bottle between the ball of the foot and the heel. Enough pressure should be applied so that a stretch is felt, but not pain.
This can be performed for as long or as short as is comfortable, ensuring it is not performed for a duration or intensity that increases symptoms.
Shoe Orthotics
Shoe inserts are available both over-the-counter and custom designed. Depending on the severity of the condition, many people try over-the-counter orthotics first and move to custom orthotics if they are not experiencing the expected improvements.
Whether custom or over-the-counter orthotics are used, the purpose is to provide external foot support to encourage improved foot positioning and biomechanics as you go about your day. These are typically easily slipped in and out of shoes, so your shoes can remain interchangeable while still receiving the same level of foot support.
Orthotics work to improve arch support, pressure distribution, cushioning, foot and ankle alignment, and overall comfort.
Orthopedic Shoes
Orthopedic shoes can provide highly individualized and effective support for a wide range of foot conditions. Designed to alleviate pain and improve foot function, they are especially helpful for conditions affecting the entire foot, including the bottom. Shoes designed for ball of foot pain or plantar fasciitis can help manage symptoms. While orthotics target specific areas, orthopedic shoes offer more comprehensive foot support. For many people, they can offer immediate pain relief, improved comfort, and better biomechanical alignment. However, the combination of orthopedic shoes with orthotics can provide the most tailored solution for addressing foot issues comprehensively.
When to See a Specialist
If you are experiencing plantar foot pain that has persisted for more than 12 weeks without notable improvement, pain that does not fully subside while not bearing weight, numbness or shooting pain through your feet or toes, or intense, sharp pain that limits your ability to stand or walk, you should see your primary care provider or a podiatrist as soon as possible for further evaluation.
Pain in the bottom of the feet is extremely common and may be a result of multiple possible factors and conditions. Depending on the severity and duration of the condition’s symptoms, you may experience relief using a singular or combination of management options including lifestyle modifications, exercises and stretches, shoe orthotics, or orthopedic shoes. However, for any severe or prolonged symptoms, as outlined above, it is imperative that you seek medical attention.
About author:
Troy Hurst, PT, DPT, is a licensed physical therapist who received his Doctor of Physical Therapy degree from Carroll University in 2017. He specializes in the treatment of orthopedic and vestibular conditions, and has been a freelance medical writer since 2018.

